You don’t feel like yourself anymore. And no one seems to take it seriously.
You tell your doctor that your brain feels foggy. That your energy has crashed. That you’re snapping at your partner or holding back tears in meetings. That the night sweats are making you dread bedtime, and your sex drive? Gone. Everything feels off, and the only answers you’ve gotten are more prescriptions, more explanations about “normal aging,” or a suggestion to just “wait it out.”
If that sounds familiar, you’re not imagining things. You’re not overreacting. And most importantly, you’re not alone.
These are the lived frustrations of women going through perimenopause and menopause. You’ve tried to white-knuckle through it. You’ve taken the supplements, overhauled your diet, done the meditations, and maybe even googled late into the night looking for something—anything—that speaks to what’s really going on inside your body.
Here’s the truth: this isn’t just a season. It’s a shift.
Perimenopause and menopause bring major changes to your hormones. Estrogen, progesterone, and sometimes even testosterone levels start to swing out of sync. That throws off your brain, your mood, your metabolism, your sleep, your heart health, and how you show up every day. It’s not just about hot flashes. It’s not just “getting older.” It’s a root cause disruption in your body’s balance—one that deserves to be addressed at the source.
At Med Matrix, we hear the same pain points in nearly every conversation:
- “I’ve seen three different doctors. They all told me this is just what happens.”
- “I don’t feel like myself, and I don’t recognize my body anymore.”
- “I want answers, not another antidepressant.”
- “Why does no one talk about this?”
You’ve done everything “right”—so why do you still feel wrong?
That’s the gap between conventional and functional medicine. Conventional medicine often treats symptoms. You’re tired, so take a stimulant. You’re angry or weepy, so here’s something for your mood. You’re not sleeping? Here’s a sleep aid.
But in functional medicine, we look at the system as a whole. That means zooming out to ask: why is this happening in the first place? Why is your body out of rhythm? And how can we help it return to balance, rather than mask the symptoms?
Hormone Replacement Therapy (HRT) can be part of that answer.
And no, we’re not talking about the outdated one-size-fits-all HRT of the past. We’re talking about a modern, individualized, functional approach that sees HRT as a tool—not the only tool, but one with real, life-changing power when used wisely.
HRT, when it’s done thoughtfully, can help restore your hormone levels, support your brain, bones, muscles, and mood, and bring your body back to a place where it feels safe and strong again. It’s not about pushing hormones at every woman. It’s about listening deeply, testing thoroughly, and collaborating on a care plan that meets your needs and aligns with your values.
You deserve more than “just deal with it.”
You deserve clean answers, restoration, and a way forward that honors your whole-body health—not just a list of symptoms.
In this guide, we’ll walk you through what Hormone Replacement Therapy really is, how it fits into a root-cause approach, what the potential benefits and risks are, and how to know whether it’s something worth exploring. All through the lens of holistic, functional care that puts you at the center of the process.
Your hormones might feel out of control. But your care doesn’t have to be.
What Is Hormone Replacement Therapy (HRT)?
If you’ve made it this far, you’re probably wondering: So what exactly is HRT? And is it just more of the same quick-fix approach, or can it actually support my body in a real, lasting way?
Let’s clear the confusion.
Hormone Replacement Therapy (HRT) is a treatment designed to bring your hormones—mainly estrogen, progesterone, and sometimes testosterone—back into a healthy balance when your body stops making them in the same amounts.
This natural drop starts in perimenopause and continues into menopause. And for many women, it doesn’t feel like a slow fade. It feels like your body hit a wall. Your energy tanks. Your mood swings. Your memory glitches. And your body starts doing things it never used to—like waking you up in the middle of the night soaked in sweat or making it feel like your skin’s crawling.
These symptoms are signals. They’re your body’s way of saying, “I’m out of balance.” That’s where HRT comes in—not to override your body or silence it, but to support it back toward a state it recognizes and feels safe in again.
The Hormones Involved
Estrogen plays a key role in regulating your menstrual cycle, mood, brain function, heart health, bones, and more. When it drops, you feel it everywhere—from your joints, to your sleep, to your libido.
Progesterone is your calming hormone. It helps balance estrogen and supports sleep, mood, and nervous system function. Without enough of it, anxiety can spike and sleep can spiral.
Testosterone (yes, women need it too) helps with muscle tone, mental clarity, motivation, and sex drive. In some cases, especially after menopause, a gentle support of testosterone may be part of someone’s HRT plan.
How It’s Delivered
HRT isn’t a one-form-fits-all approach. There are different ways to get these hormones into your body, and the method you use should depend on your symptoms, your biology, and your long-term goals. Here are the main delivery options:
- Pills: Easy to take, but for some women, oral hormones increase liver workload and aren’t ideal for metabolism or clotting risks.
- Patches: These deliver estrogen through the skin, bypassing the liver and providing a steady release.
- Gels and creams: Applied to the skin, these are a flexible and often lower-impact method—helpful for precision dosing.
- Vaginal applications: Available as creams, rings, or tablets, these target local symptoms like dryness or urinary issues without affecting your entire system.
- Pellets: Implanted under the skin, they release steady doses over time. They can be helpful for some, but carry less flexibility if symptoms or needs change.
Your delivery method isn’t just about convenience. It also impacts how your body absorbs the hormone, how stable your levels stay, and how your overall system responds. That’s why we don’t just hand you a prescription and send you home. We take your symptoms, lab work, history, and lifestyle into account before making any decision.
Bioidentical vs. Synthetic: What’s the Difference?
This question comes up a lot, and it matters—especially if you’re someone who’s tried to do things the “natural” way for a long time and feels hesitant about adding hormones back in.
Bioidentical hormones are made to be structurally identical to the hormones your body produces naturally. They’re usually derived from plant sources and compounded to match your specific hormone levels. This “look-alike” quality means your body often recognizes and uses them more efficiently, and side effects can be lower.
Synthetic hormones don’t have the same chemical structure as your natural hormones. Some women metabolize these differently or more harshly, and they may come with a different risk profile depending on what’s used and how it’s delivered.
In functional medicine, bioidentical hormones are often preferred because they align with the goal of mimicking your body’s natural rhythm rather than overriding it. But this isn’t about jumping on a trend. It’s about finding what actually works best for your body and your goals—because you’re not just trying to check a box. You’re trying to feel like you again.
This Isn’t About “Fixing” You. It’s About Supporting What’s Already There.
If anyone’s ever told you that you’re just getting older and need to accept it, please hear this:
Declining hormones aren’t a character flaw. And using HRT doesn’t mean you’re weak, broken, or taking the easy way out.
This is your health. You get to take it seriously.
The Role of Hormones in the Body: Beyond Symptom Relief
If your brain feels like it’s stuck in a fog, your moods are swinging like a pendulum, or your body aches in new places for no clear reason, you’re not imagining it.
Your hormones are more than chemical messengers. They’re the behind-the-scenes regulators of how you think, feel, move, and function. When estrogen and progesterone start to drop or fluctuate—as they do in perimenopause and menopause—your whole system can feel like it’s going off the rails.
This shift affects everything from memory to motivation, body composition to sleep, heart health to mental clarity. And it’s not just “aging.” It’s not all in your head. It’s a real biological disruption that deserves real attention.
Hormones Aren’t Just About Periods and Pregnancy
Most people were taught that estrogen and progesterone are mainly about fertility or your monthly cycle. That’s true—but it’s also deeply incomplete.
These hormones play massive roles across your entire body, and when they drop, the effects ripple through every system.
Let’s break it down:
1. Brain Health and Memory
Estrogen supports brain function at a cellular level. It helps with blood flow to the brain, supports memory, and protects neurons. That’s why many women describe memory problems, fuzzy thinking, or trouble focusing as their hormones shift.
Progesterone also has calming effects on the brain. It interacts with GABA receptors, which help regulate anxiety and promote a sense of ease.
When these hormones dip, it’s no wonder you feel wired but tired, forget what you were saying mid-sentence, or can’t gather your thoughts in the way you used to.
2. Cardiovascular Function
Your heart isn’t separate from your hormones. Estrogen helps keep blood vessels flexible and supports healthy cholesterol balance. It also affects how your body regulates inflammation—a key factor in long-term heart health.
When estrogen starts to drop, those protections fade. That’s one reason the risk of heart concerns can rise after menopause. But most conventional care doesn’t connect the dots until after something shows up in labs or symptoms.
At Med Matrix, we believe in getting ahead of that curve, not just reacting after the fact.
3. Bone Density and Strength
Estrogen tells your body, “Keep the bones strong.” It supports the activity of cells that build bone and helps slow down the ones that break it down too quickly.
Without enough estrogen, your bones can lose density faster than they build it. That sets the stage for fragility and higher risk of fractures years down the line.
This isn’t just about the future either. Less estrogen means joint pain, backaches, and a body that starts to feel more breakable than it used to. You may find yourself moving differently or hesitating to lift things that once were easy.
4. Muscle Mass and Physical Resilience
If you’ve noticed that you’re gaining fat more easily or losing muscle even while exercising, hormones could be part of the reason. Estrogen plays a role in how your body uses insulin, builds muscle, and burns fat.
Testosterone also contributes to muscle tone and energy. While less talked about in women’s health, it matters more than most people realize—especially as you hit midlife.
Your contour changes. Your stamina drops. It’s not laziness. It’s physiology in flux.
5. Mood, Sleep, and Emotional Regulation
Night sweats, restless sleep, and feeling like you’re on the verge of tears every other day? That’s not just “stress.” That’s a hormonal disruption in full swing.
Estrogen helps boost serotonin and reduce cortisol (your body’s main stress hormone). Progesterone soothes your nervous system and helps cue restful sleep.
When those levels plummet or become unpredictable, it messes with your emotional stability. You’re not just moody—you’re on a rollercoaster your body didn’t choose to ride.
6. Energy and Vibrancy
This is where so many women get stuck. You’re doing all the things—eating clean, exercising, taking your supplements—but you still feel sluggish. Heavy. Like the life force just isn’t there anymore.
That’s not you failing. That’s your body signaling.
Hormonal balance supports how your mitochondria (your energy factories) function, how your cortisol levels stay in check, and how resilient you feel moving through life. You can eat kale and meditate all day, but if your hormones are in chaos, your energy will still lag behind.
When Balance Breaks, You Feel It in Every Direction
The decline or dysfunction of hormones doesn’t just show up in lab results—it shows up in your lived experience.
- That sudden burst of anger over something small? That’s hormonal.
- The urge to cry without knowing why? Hormonal.
- That feeling like life is moving forward without you, like you’re watching it from the sidelines? Also hormonal.
This isn’t about being dramatic. It’s about being honest.
You deserve more than a pat on the head and a sleep aid. You deserve clarity about what’s happening in your body and real pathways to support it through a transition that affects every cell you live in.
This Is the Root, Not the Side Effect
Hormones aren’t just the reason you’re uncomfortable. They’re the root signaling that your body is in transition, out of sync, and needing support to find its rhythm again.
That’s why in functional medicine, we use HRT not to patch up pain points but to help reinstate your body’s natural messages. We treat estrogen, progesterone, and sometimes testosterone levels with the care and precision they deserve—because they anchor your mood, metabolism, cognition, and structure. This is bigger than hot flashes. It’s whole-life restoration.
You shouldn’t have to apologize for wanting to feel like you again.
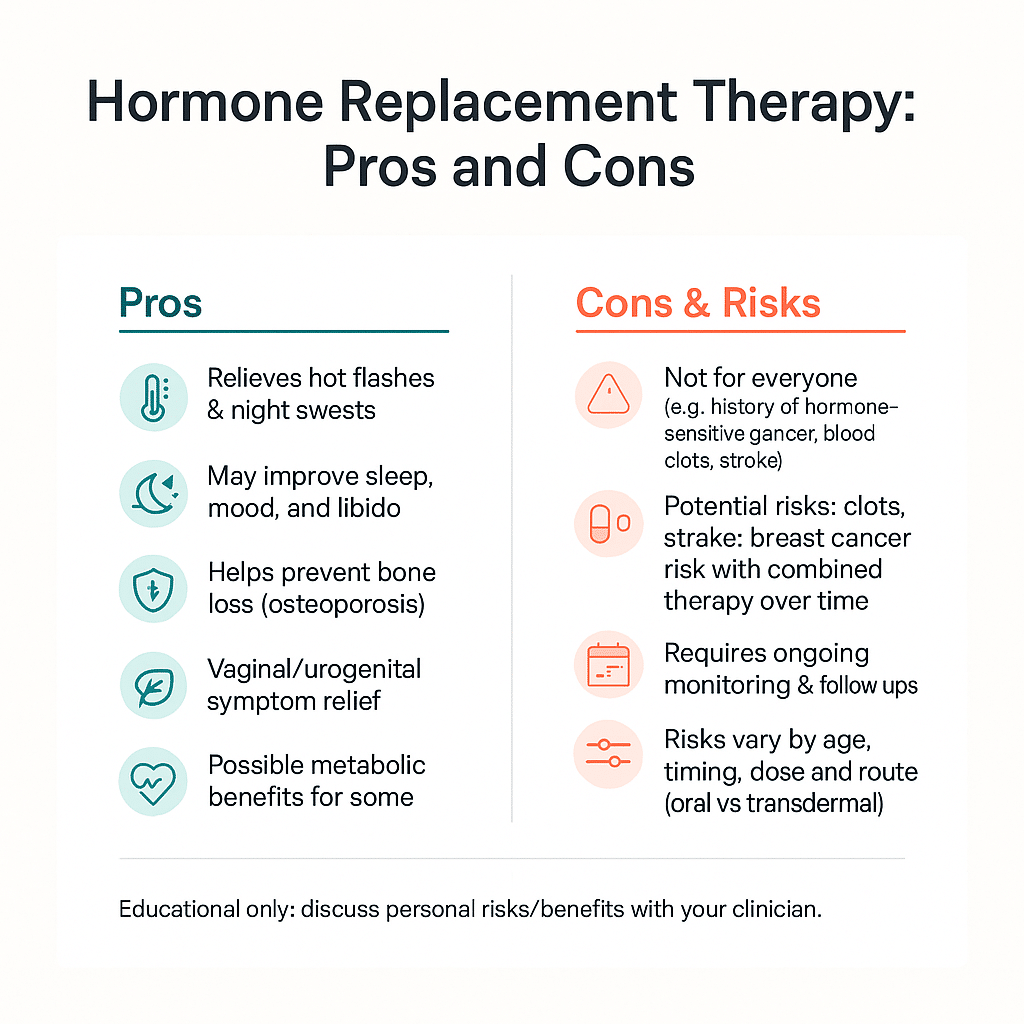
Pros of Hormone Replacement Therapy: Comprehensive Benefits
If you’re here, it’s probably because the idea of feeling like yourself again doesn’t sound like a pipe dream. It sounds like a need. A basic, non-negotiable need.
That’s not too much to ask. That’s the baseline you deserve.
When used as part of a whole-body, functional approach, HRT has the potential to bring real relief—not just from the “classic” menopause symptoms, but from the way those symptoms ripple through every part of your life.
This Isn’t Just About Hot Flashes (Though It Helps Those Too)
Let’s start with the obvious: HRT can help stop the intense, sweaty chaos your body’s been putting you through. For many women, this means:
- Hot flashes ease or disappear
- Night sweats stop waking you up
- Vaginal dryness improves, making intimacy feel comfortable again
But those are just the surface signs. What’s underneath is often even more important—because when your sleep normalizes, when you’re no longer jolted awake drenched in sweat, when you’re no longer bracing for another flush at work or worrying about intimacy with your partner, your day-to-day life becomes manageable again.
It’s not about vanity. It’s about stability.
Bone Strength and Muscle Preservation
One of the most overlooked advantages of HRT is how it helps protect your structural strength.
Estrogen plays a key role in building and maintaining bone density. When it drops, your bones start to lose mass faster than your body can rebuild. Over time, that can lead to joint pain, brittle bones, and higher risk of fractures.
HRT helps slow that process. It tells your body, “Keep that scaffolding strong.” And when your bones are stronger, you feel more confident moving through daily life without worrying about injury.
Alongside that, you may notice it’s easier to maintain muscle mass. That matters for your metabolism, your balance, your energy, and your ability to do the things you love—whether that’s lifting a grandchild, hauling groceries, or taking your usual walk without feeling wiped out.
Support your body so it supports you.
Brain Health and Mental Clarity
Ever feel like your mind is wrapped in cotton? Like the word you’re trying to find is stuck inside your mouth but won’t come out?
That fog isn’t just aging. It’s often hormone related. Estrogen is involved in blood flow, neurotransmitter function, and cellular protection in the brain. When it dips, lots starts to misfire.
Starting HRT earlier—especially during perimenopause—may help protect cognitive clarity and mental focus. That means less distraction, less forgetfulness, and more of that clear-headed confidence you haven’t felt in a while.
Your thoughts matter. Let’s support the system that helps organize them.
Heart Health Gets a Boost
Your hormones and your heart are deeply connected. Estrogen influences blood vessel flexibility, supports healthy cholesterol ratios, and plays a role in inflammatory balance in the cardiovascular system.
When estrogen drops, women’s heart risks start to rise. That’s not about fear—it’s about awareness. Using HRT as part of a multifaceted care plan may support cardiovascular health, especially when started closer to menopause and tailored to your individual risk factors.
You shouldn’t have to wait for a scare to begin caring for your whole system—prevention is power.
Mood and Emotional Resilience
When people say you’re just moody or hormonal, they often miss what that actually feels like to live inside.
The racing thoughts. The sudden tears. The irritability that shows up before your brain realizes you’re angry. The ups and downs that make you distrust yourself emotionally.
Estrogen and progesterone both play a role in regulating mood, by boosting feel-good chemicals like serotonin and calming the stress response. With appropriately dosed HRT, many women notice a steadying of the emotional rollercoaster. Anxiety calms down. Rage feels less volatile. Sadness doesn’t hit quite so hard or so often.
This isn’t about numbing you. It’s about grounding you.
Sleep That Actually Restores You
When was the last time you slept through the night and woke up feeling rested?
HRT can help restore your natural sleep-wake signals. By stabilizing hormone levels, it can reduce night sweats and help re-regulate the brain chemicals that signal when it’s time to rest.
Wouldn’t it be nice to fall asleep without a fan, wake up without a soaked pillow, and feel like you actually got rest instead of surviving another night?
You need real sleep, not just more melatonin.
Benefits for Women Over 50 and During Perimenopause
If you’re already in menopause, it’s not too late. And if you’re in perimenopause, you’re actually in a key window where HRT may do even more to support long-term well-being.
Starting HRT earlier—not waiting until everything crashes—can potentially:
- Help preserve brain and cardiovascular health
- Make the transition through menopause less rocky
- Protect bone and muscle before decline accelerates
- Give you the chance to feel anchored, rather than dragged along by symptoms
Even if you’re over 50, the right functional medicine strategy can still make HRT viable and impactful when done with proper testing, monitoring, and individualized care.
This isn’t about turning back the clock. It’s about making the years ahead feel like yours again.
A Tool for Restoration, Not a Band-Aid
Every woman’s experience is different. And not every woman will choose or need HRT. But for those who do, when done right, HRT can be about so much more than symptom relief.
It can be about support. Strength. Sleep. Sanity. And a return to feeling like you can actually show up for your own life—not in survival mode, but in stability.
You’re not chasing your 30s. You’re reclaiming your right now.
And if that means exploring HRT as part of your care plan, we’ll walk with you every step of the way—because your body’s not broken. It’s crying out for balance. And that is absolutely something worth listening to.
Cons of Hormone Replacement Therapy: Understanding the Risks and Side Effects
It’s okay to have questions. It’s okay to feel torn.
If you’re here, chances are, you’ve already heard the whispers. Blood clots. Breast cancer. Mood swings. You’ve probably googled things late at night and ended up scared, overwhelmed, and more confused than before. Maybe a doctor mentioned risks without much explanation. Maybe someone dismissed your concerns entirely. Either way, you deserve better than vague warnings or rushed answers.
Let’s be honest about this: Hormone Replacement Therapy comes with risks. But those risks, just like the benefits, have context. And in functional medicine, context is everything.
What Risks Are We Talking About?
When people talk about the “dangers” of HRT, this is usually what they mean:
- Increased risk of blood clots (including deep vein thrombosis)
- Stroke risk (particularly with certain delivery methods or in older age groups)
- Possible link to specific cancers (such as breast or uterine, depending on hormone type and duration)
That sounds serious—because it is. But here’s where it gets more nuanced.
The Details Matter
These risks don’t apply the same way to every woman. Age, delivery method, hormone type, dosage, duration, and personal health history all affect what level of risk you’re actually dealing with.
- Age: The risk profile shifts based on when you start HRT. Starting closer to menopause (typically before age 60 or within 10 years of your last period) tends to be associated with fewer adverse risks—especially in healthy women.
- Delivery method: Oral estrogen can impact the liver and increase clot risks, while transdermal methods like patches or gels typically bypass this concern.
- Hormone type: Synthetic progestins used in traditional HRT have shown a different risk pattern than bioidentical progesterone. The choice here really matters.
- Personal history: If you’ve had certain health events in the past—like breast cancer, strokes, or clotting disorders—HRT may not be the best fit unless carefully supervised by the right team.
This isn’t about scare tactics. It’s about informed decisions.
The Most Common Side Effects (and What They Feel Like)
Not every reaction is life-threatening. Sometimes HRT just doesn’t feel right at first—your body may need time to adjust. Here’s what some women notice early on:
- Headaches, especially if estrogen levels shift too quickly
- Nausea or bloating, depending on how your gut responds to oral hormones
- Breast tenderness, especially as tissues re-sensitize to hormone changes
- Mood swings or increased anxiety (often due to imbalances in progesterone or estrogen ratios)
- Spotting or irregular bleeding, particularly early on or with improper dosing
These symptoms are real. And they don’t mean you’re doing it wrong. They mean your body is speaking up. We don’t ignore that. We listen, test, and adjust.
Here’s What We Hear from Women All the Time:
- “I’m afraid of starting something that I can’t control.”
- “What if I feel worse on hormones than I do now?”
- “I don’t want to increase my cancer risk just to stop sweating at night.”
These concerns are valid. You have every right to weigh the risk of taking hormones. But you also deserve to weigh the risk of not treating hormonal disruption.
Untreated menopause symptoms aren’t just uncomfortable—they can affect your bones, your heart, your brain, your muscles, and your safety. In some cases, the long-term risks of no treatment at all may be greater than the carefully guided use of HRT.
What Does “Functional Medicine Safe” Look Like?
In conventional care, HRT might mean a one-size-fits-all pill. In functional medicine, that’s never the approach. Safety starts with personalization. Here’s our framework:
- Thorough screening: We run labs, review history, check family risks, assess your current state, and match your body’s readiness with the right approach.
- Bioidentical preference: Whenever appropriate, we use hormones that are chemically identical to your body’s own—not synthetic types shown to have higher risk profiles.
- Transdermal delivery: Creams, gels, or patches bypass the liver and often reduce clotting risk. This is safer for many women, especially those over 50.
- Adding progesterone for balance: If you still have a uterus, you need progesterone to offset estrogen’s effect on the uterine lining. Bioidentical progesterone is often better tolerated and more protective than synthetic versions.
- Titrated dosing: We don’t blast your system. We start with the lowest effective dose, monitor your response, and fine-tune as needed based on lab and symptom feedback.
- Regular monitoring: We don’t just “set it and forget it.” HRT needs ongoing check-ins through labs, conversations, and symptom tracking to make sure it’s helping, not harming.
This isn’t passive care. This is partnership.
It’s Okay to Take Your Time
Feeling scared or hesitant doesn’t mean you’re weak. It means you care about your body and want to make a wise choice. We’re not here to talk you into anything. We’re here to walk alongside you through real conversations that make room for both hope and honest caution.
Maybe HRT is right for you. Maybe it isn’t. But either way, you deserve to have the full picture—not just a generic warning or a quick “you’ll be fine.”
Real care doesn’t ignore risk. It works within it.
And that’s what we do together—build a plan that helps you feel safe, supported, and in control of your care again. You don’t have to settle for overwhelm. You don’t have to gamble with your well-being.
This is your decision, and we’ll help you make it with eyes wide open.
Timing and Individualization: Starting HRT in Perimenopause vs. After Menopause
You’ve probably asked yourself: Is it too early? Is it too late? Or is now the right time?
When it comes to Hormone Replacement Therapy, timing is everything. Not just for how well HRT works—but for how your body responds, how safe the therapy is, and how lasting the benefits can be.
Let’s break down the difference between starting HRT in perimenopause versus waiting until after menopause, and why your body’s current state matters more than your birthday.
The Critical Window: Why Sooner Can Be Smarter
One of the phrases that comes up in both research and clinical conversations is something called the “critical window hypothesis.” Here’s what that means in plain language:
There’s a window of time—usually during perimenopause or early menopause—where starting HRT may offer the most benefit and the least risk.
When your hormones haven’t been gone for too long, your body still “remembers” how to respond to them. So reintroducing hormones like estrogen, progesterone, or even testosterone can feel more natural and rhythm-based. Your brain, heart, bones, and nervous system are still tuned in—and that makes support more effective.
Wait too long, and the window starts to narrow.
This doesn’t mean you missed your chance. But it does mean we need to approach things more slowly and intentionally later in life.
What Changes Between Perimenopause and Post-Menopause?
Perimenopause is often the most chaotic time. Your hormones aren’t just low—they’re unpredictable. One month you might feel fine, the next you’re battling insomnia and rage out of nowhere.
Starting HRT during perimenopause can help stabilize that rollercoaster. It doesn’t stop menopause from coming. But it may soften the ride, make the transition more manageable, and help prevent some of the downstream effects—like bone loss and cognitive shifts—that kick in later.
Once you’re in full menopause (meaning it’s been at least 12 months since your last period), your hormone levels have typically flatlined. At that point, HRT often serves more as restorative support than stabilization. This is still incredibly valuable, both for symptom relief and long-term health, but the way we dose and monitor may need to shift.
This is why personalization matters so much.
What Makes Someone a Good Candidate At Each Stage?
There’s no one-size-fits-all checklist. But here’s a general framework our team considers when helping women decide when (and if) to start HRT:
If You’re in Perimenopause:
- You still have a period, but it’s becoming irregular
- You’re experiencing new or worsening symptoms like night sweats, mood changes, low libido, or brain fog
- You feel like your normal tools (sleep, diet, exercise) aren’t cutting it anymore
If this is you, early intervention could make a big difference. Supporting your hormones now may help ease the eventual transition and reduce long-term health shifts related to bone, brain, and heart function.
If You’re Already Post-Menopausal:
- It’s been over a year since your last period
- You still struggle with symptoms (sleep issues, vaginal changes, low energy)
- You’re concerned about bone loss, heart health, or brain clarity moving forward
If this sounds like where you’re at, there are still strong reasons to explore HRT. We just tailor the approach more conservatively, using lower doses, safer delivery methods, and more frequent check-ins to respect where your body is now.
The Functional Medicine Approach to Timing
We never just look at the calendar. We look at your whole health history.
In functional medicine, we ask deeper questions:
- What symptoms are you dealing with—and what are they telling us?
- What are your current hormone levels looking like?
- What’s happening with your gut, liver, immune system, and lifestyle?
- Are there early warning signs of bone or cognitive change?
- What are your health goals—strength, stability, sleep, mental clarity?
Your care plan should reflect those answers, not a generic protocol.
Tailoring HRT: How We Match Treatment to the Whole You
Starting HRT isn’t just about adding estrogen. It’s about understanding where and why your body is out of balance.
That means we take into account:
- Hormone testing: Looking at estrogen, progesterone, testosterone, and other markers across your cycle or timeline
- Metabolic health: Blood sugar, inflammation, cardiovascular profiles
- Liver and detox pathways: How well your body processes and clears hormones
- Emotional wellness: Assessing stress, anxiety, mood history, and nervous system load
- Lifestyle and routine: Sleep, exercise, nutrition, relationships, and stress patterns
Based on that picture, we decide together:
- When the time is right to start
- What type and form of hormones are best (e.g. patch, cream, oral, vaginal)
- How frequently to monitor and adjust
This kind of detailed, therapeutic matching is what gives HRT its power—and what keeps it safe within a functional medicine care model.
Bottom Line? This Isn’t a Race. It’s a Relationship.
You don’t have to rush into HRT. You also don’t need to keep waiting just because no one’s taken your symptoms seriously yet.
Whether you’re just starting to feel off or have been in menopause for years, the timing can still be right—as long as it’s right for you.
Your hormones are unique. Your timeline is too.
And with the right support, there’s still time to feel stronger, clearer, and more stable in your body again. Not by forcing it back into a past version—but by listening to what it needs now, and responding with care, precision, and partnership you can trust.
We don’t guess. We listen. We test. And we tailor—every step of the way.
If you’re ready for answers instead of more waiting, this could be the right time to begin.
Safety Measures, Monitoring, and Duration of Therapy
This isn’t “set it and forget it” healthcare. HRT done right takes partnership, precision, and real-time feedback from your body.
If you’ve been piecing together answers through online searches, blog posts, and half-hearted doctor visits, you’re probably wondering the same thing so many of our patients ask us:
“I want to feel better, but how do I know this won’t make things worse?”
The answer: safety isn’t just a precaution. It’s a process. A smart, structured, and proactive process that keeps your hormones working for you, not against you.
Step One: Start With the Right Foundation
Before HRT begins, we take inventory of your internal world. That means:
- Comprehensive lab work: We look at hormone levels, thyroid function, vitamin D, inflammation markers, cardiovascular indicators, and metabolic health. This tells us where you stand and what your body needs now—not 10 years ago.
- Personal and family history: Clues about clotting risks, cancer history, or past procedures matter. They shape the plan from day one.
- Symptom mapping: We match what you’re feeling to what your lab data shows. The goal is clear alignment between symptoms and the therapy you receive.
You’re not signing up for blind treatment. You’re entering a relationship with your care team built on transparency and trust.
Personalized Dosing: No Two Bodies, No One-Size Plan
This is where so many conventional approaches fall short. A generic dose, given without context, can leave you feeling off or even worse than before.
We believe in titrated dosing. That means:
- Start low, go slow: We introduce hormones at the minimal effective dose, then adjust based on how you respond. Not everyone needs a full-on hormone overhaul. Some just need a nudge to restore balance.
- Restoration, not flooding: We’re helping your body remember its rhythm—not trying to blast it into shape with high doses that your system can’t handle.
- Biofeedback leads the way: We track your sleep, mood shifts, energy, libido changes, and more to continuously fine-tune as needed.
Good HRT doesn’t mask. It harmonizes.
Ongoing Monitoring: Your Safety Net
You deserve more than a refill prescription every 6 months with no follow-up.
Safe HRT means repeat lab testing and consistent communication. Here’s what that looks like:
- Hormone panels: Regular testing (usually every 3 to 6 months early on) helps us make sure your levels are stable and in the right range for you.
- Liver, thyroid, and metabolic markers: We track how your body is processing and responding to treatment.
- Symptom review: You tell us how you’re feeling day to day. That information matters as much as your labs.
- Adjustment sessions: If something’s off—a mood swing comes back, sleep gets weird, a side effect shows up—we revise the plan. Together.
Monitoring isn’t about micromanaging. It’s about responsiveness. Your body changes. We shift with it—not six months too late, but in real time.
Duration of Therapy: How Long Is “Too Long”?
Another popular question we hear: “How long will I be on this?”
There’s no one answer, because it depends on your symptoms, your goals, and how your body responds to therapy.
But here’s how we approach it:
- Short-term support (a few years): For some women, HRT is the bridge that gets them through the thick of the transition. Once stability returns, they may explore tapering off.
- Long-term use (10+ years): Some women, after carefully considering risk and benefit, choose to stay on a low, maintenance dose—especially to support bone, brain, and heart health as they age. With appropriate surveillance, this can be a safe and beneficial choice.
- Flexible duration: Nothing is set in stone. We evaluate every 6 to 12 months to determine whether staying on HRT still makes sense physically, emotionally, and functionally.
We build your plan to evolve with you, not trap you.
Tapering Off (If and When You Decide To)
If the time ever comes to reduce or stop HRT, we do it gently, with support and strategy:
- Gradual dose reduction: Your body has been supported by these hormones. A sharp drop can feel like a shock, so we reduce slowly to minimize disruption.
- Symptom tracking during the taper: We keep reviewing how you’re feeling so we can step back up if things go sideways.
- Adding non-hormonal support: Nutritional changes, targeted supplements, and other therapies can help your body hold steady even as hormone levels come down.
This isn’t ripping off the band-aid. It’s walking you off the bridge you’ve built.
Integrating Lifestyle and Whole-Body Support
Hormones aren’t magic pills. They work best as part of a functional health plan that supports all the body systems involved in balance. This is why we pair HRT with:
- Therapeutic nutrition: Foods that optimize liver detox, blood sugar, and hormone pathways
- Movement routines: Resistance training for bone and muscle, gentle cardio for heart and mood support
- Stress reduction: Nervous system support through sleep hygiene, breathwork, or emotional coaching
- Supplementation: Key nutrients like magnesium, omega-3s, B vitamins, and adaptogenic herbs for added resilience
You’re never just given a script and sent home. We’re treating the whole picture—because your hormones are only one headline in your health story.
Bottom line: Safe HRT isn’t just about taking the right drug. It’s about walking the right path with the right guide.
You deserve a care team that monitors, modifies, and moves with your body—not one that forgets you exist until your yearly checkup.
We see the whole you. We listen for feedback. We don’t assume. And we make sure your hormones are part of your support system—not another thing dragging you down.
If you’re craving stability, clarity, and a care strategy built on mutual trust, this is how you get there—patient by patient, plan by plan.
Alternatives and Complements to Hormone Replacement Therapy
Hormone therapy isn’t the only path forward.
For many women, HRT becomes part of a well-rounded plan for managing perimenopause or menopause. But for others, it may not feel like the right fit—or it might only address part of what’s going on. That’s where non-hormonal options step in.
Maybe you’re not ready for hormones. Maybe you can’t use them because of past health conditions. Or maybe you’re already on HRT and still feel like something’s missing.
Good news: There are other tools to help your body reset and realign.
The Functional Medicine Approach: More Than “Take This Instead”
This isn’t about picking a supplement off a shelf and hoping for the best. In functional medicine, we look at the root causes disrupting your hormone balance—and work from there.
What’s throwing your system off? Is it poor detox? Chronic stress? Blood sugar instability? Sleep deprivation? Inflammation? These are the puzzle pieces we examine, because you don’t fix hormones by only focusing on hormones.
Let’s talk through non-hormonal paths that actually support your body—whether you’re avoiding HRT entirely or using these alongside it for fuller support.
1. Lifestyle Modifications: Foundational First Steps
These aren’t just generic wellness tips. They’re the daily habits that help your body regain hormonal rhythm.
- Sleep consistency: Go to bed and wake up around the same time. Quality sleep keeps cortisol steady and supports hormone regulation overnight.
- Strength-based movement: Resistance training helps preserve muscle, support metabolism, and improve insulin sensitivity—all key during midlife changes.
- Stress reduction practices: Try breathwork, walking in nature, or guided meditations. Managing stress calms cortisol, which can otherwise wreak havoc on your hormones.
- Daily sun exposure: Vitamin D plays a role in hormone synthesis and mood regulation. A few minutes outdoors can help reset circadian rhythms too.
Simple doesn’t mean ineffective. These habits are the bedrock of hormone-friendly living, whether you’re using HRT or not.
2. Targeted Nutrition: Food That Talks to Your Hormones
You can’t out-supplement a poor diet. But you can design meals that actively communicate safety and stability to your hormonal system.
- Healthy fats: Avocados, olive oil, nuts, and seeds feed your endocrine system and support cholesterol balance (which helps hormone production).
- High-fiber vegetables: Cruciferous veggies like broccoli, cauliflower, and kale support estrogen metabolism and liver detox pathways.
- Protein with each meal: This helps balance blood sugar, preserve lean mass, and support neurotransmitter production.
- Reduce highly processed foods: Sugar, additives, and preservatives drive inflammation, which can pull your hormones further out of sync.
Eat in a way that tells your body, “I’m safe. You can stabilize now.”
3. Herbal and Natural Supplements: Gentle but Targeted Support
We often hear: “Are there herbs that actually work?”
The answer? Yes—but they have to be used correctly, at the right dose, and matched to your specific symptoms. Here’s a framework we might draw from based on common symptom patterns:
If Sleep is a Struggle:
- Magnesium glycinate or threonate
- L-theanine to support calm
- Adaptogens like ashwagandha or rhodiola (depending on your cortisol pattern)
If Mood is Unpredictable:
- Maca root for energy and emotional resilience
- SAM-E or 5-HTP for mood support (used cautiously and never combined with SSRIs)
If Hot Flashes are Frequent:
- Black cohosh for vasomotor symptoms
- Evening primrose oil or flaxseed for phytoestrogens
- Sage tea or tincture for night sweats
Important: Not all supplements are safe for everyone. This is where working with a qualified practitioner matters. We review your full health history, medications, and goals before recommending any herbs—even the “natural” ones.
4. Non-Hormonal Medications: Pharma Can Still Have a Role
In some cases, prescription medication might be part of your toolkit, even if you’re not using hormones. These aren’t about throwing pills at problems. They’re about targeted relief while we address the root system-wide causes.
Here are a few classes your provider might consider:
- Antidepressants (SSRIs/SNRIs): Low-dose options can help manage hot flashes and mood swings for women who aren’t candidates for HRT.
- Gabapentin: Originally used for nerve pain, it has shown effectiveness in reducing night sweats and improving sleep quality.
- Clonidine: Sometimes used to reduce hot flashes, especially in women with high blood pressure.
You’re not “giving up” if you explore medications. The goal is to relieve suffering—while still working toward long-term stability through nutrition, sleep, and stress support.
5. Integrative Approaches: Supporting the Whole System
Outside of food, herbs, and medication, other therapies can help strengthen your body’s foundation during this hormonal shift.
- Acupuncture: This can support nervous system regulation, reduce hot flashes, and improve sleep by calming the parasympathetic system.
- Pelvic floor therapy: Especially for women navigating vaginal dryness or urinary issues, targeted pelvic therapy can increase circulation and tissue health.
- Mind-body coaching: Emotional processing, trauma release, and somatic support can reduce internal stress load that contributes to hormonal imbalance.
Your body doesn’t compartmentalize stress, food, sleep, or emotion—so neither should your plan.
So What’s the “Right” Way Forward?
There is no right answer for everyone. The best strategy often includes a combination: maybe HRT alongside nutrition upgrades and stress support. Maybe herbal therapies first, with the option to introduce hormones later. Or maybe just small but meaningful shifts in your daily routine that add up to real relief.
Here’s what matters most: that your plan is built for YOU.
We don’t prescribe based on trends or settle for temporary fixes. We co-create a care map that honors:
- Your unique symptoms
- Your risk profile
- Your goals and values
- Your body’s signals
And we stay flexible—because what works today might need adjusting tomorrow. That’s real care.
You don’t have to pick one magic fix. You get to build a layered support system that works at every level—from mood to mitochondria.
If you’re ready for real support that meets you where you’re at, we’re here to craft it with you—step by step, system by system.
When to Consult a Hormone Specialist: Navigating Your Treatment Journey
You know something is off, but no one’s helping you figure out why.
Maybe you’ve been told “your labs look fine.” Or maybe you’ve been handed sleep meds, mood stabilizers, or told to “just give it time.” But deep down, you know this isn’t in your head. It’s in your hormones. And it’s time someone looked at the whole picture—not just pieces of it that passed a blood test or fit into a rushed 10-minute appointment.
So how do you know if you need a hormone specialist? And what does it even look like to work with someone who actually sees the full you, listens deeply, and understands how to guide you through hormone changes with clarity and care?
Let’s start with the signs that it’s time to seek help.
These are the signals we hear from patients over and over—the red flags your body may be waving, even if no one else is noticing:
- Your symptoms are getting louder, not better. You’ve tried the lifestyle stuff. You’re eating better, moving more, prioritizing sleep—but it’s not shifting the constant fatigue, crashing mood, brain fog, or hot flashes.
- You feel emotionally unstable in ways you don’t recognize. You’re quicker to cry, more irritable with loved ones, or just not feeling like yourself. And you know it’s not just “stress.”
- Your periods are changing fast—or have disappeared. Bleeding patterns shifting quickly? Spotting? Wild PMS symptoms? Or no cycle at all for over a year? These aren’t just quirks. They’re hormone cues.
- Your sleep is disrupted, even though you’re exhausted. Night sweats. Wired but tired. Waking up drenched, then dragging by day. Hormonal imbalance could be behind the chaos.
- You’ve been dismissed—or told it’s just aging. You know that “normal” aging should not feel like your life being replaced by someone else’s sluggish, overwhelmed body and mind.
If any of that sounds like you, yes—this is a good time to consult a hormone specialist.
But not just any hormone specialist. Here’s what to look for.
Finding the right person to walk this path with you is just as important as deciding to seek help in the first place.
In functional medicine, we do this differently. Instead of rushing to write prescriptions, we:
- Listen before we test. Your story tells us what your labs might not. We listen for timing, shifts, stress patterns, and emotional toll—not just symptom checklists.
- Run deeper labs, not just routine panels. We look at hormone patterns (not just single spot numbers), detox capacity, gut health, inflammatory markers, and more. You’re complex. So is your care.
- Customize treatment to your whole body. We don’t just throw estrogen at you. We decide, together, what you actually need—whether that includes HRT, herbal support, lifestyle shifts, or a combination of options.
- Track your progress with real data and real conversations. No “set it and forget it.” We circle back, recheck labs, listen to your feedback, and adjust your plan as your body evolves.
So how do you find this kind of care?
How to Find a Hormone Therapy Provider Aligned with Functional Medicine
Not every provider offering hormone therapy practices from a root-cause lens, and not every functional medicine provider specializes in hormones. You want both. Here’s how to search with clarity:
Signs they could be the right fit:
- They offer comprehensive hormone testing (not just basic estrogen levels).
- They review your full health picture—history, symptoms, lifestyle, and goals—before suggesting therapy.
- They use bioidentical hormones when appropriate. Not because it’s trendy, but because your body often handles them better.
- They create ongoing monitoring plans. Including regular labs, response tracking, and revisits—not once-a-year check-ins.
- You feel heard and in control, not talked down to. If you feel silenced, bulldozed, or rushed, that’s a no.
It should feel like partnership, not prescription.
What Collaborative, Individualized Care Feels Like
If you’ve only ever had a doctor skim your chart and hand you a med, this next part might sound foreign. But it shouldn’t.
Working with a functional hormone specialist means co-creating your treatment plan with someone who treats you like the expert of your own body.
Here’s what that looks like in practice:
- Your symptoms are taken seriously, even if your labs are “normal.”
- You’re involved in choosing your therapy. We walk through benefits, side effects, delivery methods, and alternatives based on your lifestyle and values.
- Your hormone doses are personalized and adjusted over time. We don’t set it once and cross our fingers. We observe and respond.
- You feel safe to ask questions, bring concerns, and name your fears. Because you’re not just a patient. You’re a partner in your care.
This is what real care looks like. Thoughtful. Responsive. Rooted in respect.
You don’t have to figure this out alone.
No more guessing. No more googling in circles at 2am. No more being told it’s all in your head.
If you’re even wondering whether hormone therapy might help, it’s worth starting the conversation. Not with someone who sees you as just another menopausal woman—but with a provider who sees the complexity, the frustration, the strength, and the potential inside you right now.
The goal isn’t perfect health overnight. It’s steady support. Restored balance. And a mind-body partnership that lasts.
If you’re ready to get back to feeling like yourself—and want a care plan that treats the whole you—it starts with finding the right specialist and asking the right questions.
Conclusion: Empowered Decision Making with Holistic Hormone Health
You’re not overreacting. You’re responding to a body that’s calling out for change.
That inner nudge you’ve felt—the one that says “this can’t be all there is”—you can trust that. It’s not just hormones wreaking havoc. It’s a wake-up call for deeper support. For a kind of care that doesn’t dismiss your symptoms, downplay your struggles, or throw pills at your pain without explanation.
This guide hasn’t been about convincing you to say yes or no to Hormone Replacement Therapy. It’s been about helping you actually understand what HRT is, what it does, when it’s useful, and what to weigh as you consider whether it’s the path for you.
You’ve learned that your hormones touch every corner of your health—your brain, bones, heart, muscles, sleep, mood, and energy. That what you’re going through isn’t “just aging” or “just stress.” It’s a systemic change that deserves to be met with real options and honest support.
And yes, you’ve seen that HRT has pros and cons. Like any therapy, it’s not perfect. But when done through a functional, root-cause lens—with thoughtful timing, bioidentical hormones, regular monitoring, and personalized dosing—it can radically change what life looks like from the inside out.
Even more importantly, you now know this isn’t about fixing you. It’s about supporting you.
It’s about finally feeling heard when you say, “I don’t feel like myself.” It’s about having a care team who believes you—even when the labs are “normal.” It’s about choosing a path that respects your values, your history, and your right to feel good in your body again.
You don’t have to keep settling. You don’t have to keep guessing.
If you’re still unsure whether HRT is right for you, that’s okay. You don’t have to rush. But you do deserve full access to information, safe ways to explore what your options are, and guidance that sees your whole picture—not just a single lab result or a passing hot flash.
Next Steps? They’re Yours to Take.
- Maybe it’s booking a lab review to see where your hormones really are.
- Maybe it’s talking to a provider who won’t dismiss your symptoms or railroad you into one choice.
- Maybe it’s starting HRT with thoughtful support.
- Or maybe it’s choosing lifestyle and nutrition steps first while keeping hormones on the table.
All of those are valid. All of them are real. All of them honor your right to choose.
You’re allowed to pursue wellness without apology. You don’t need to hit rock bottom before doing something about what your body’s been trying to tell you.
And if you’re looking for a place to start—not just another blog post, but a partner in this journey—you’re in the right place. We’ve helped women just like you untangle the mess of contradictory advice, find clarity in their symptoms, and make powerful, sustainable choices for the way they feel today, and the way they want to live tomorrow.
Your story deserves real solutions—not dismissal.
If you’re ready to stop guessing and start healing, this is your moment.
Your hormones might be in chaos, but your care doesn’t have to be. With the right lens, the right tools, and the right team, you can move through this chapter not just surviving—but steadily rebuilding your strength, your rhythm, your clarity, and your joy.
This is your body. This is your life. You get to feel at home in both.